[6 min read]
In this article:
- Chronic venous insufficiency (CVI) is a disease that occurs when veins in your legs are damaged and can’t manage blood flow as well as they should. With CVI, blood pools in your leg veins, increasing the pressure in them and, in turn, on your vascular system.
- Chronic swelling of the legs and ankles, particularly after sitting or standing for longer periods, night time leg cramps, or reddish-brown skin stains on the legs are common CVI symptoms.
- If you suspect that you have CVI, it's important to see a physician as soon as possible to prevent additional, serious health risks.
- A Providence Swedish vascular surgeon shares more guidance for recognizing and managing the condition.
According to news reports, President Donald Trump was recently examined for swelling in his legs and diagnosed with chronic venous insufficiency (CVI), a condition that compromises the ability of valves in the veins to control blood flow, allowing blood to pool in the veins. It’s a common problem affecting an estimated 25 million people in the United States. Symptoms can include swelling in the ankles or lower legs, cramping, varicose veins and darkening of the skin, otherwise known as skin staining. Risk for chronic venous insufficiency increases with age. CVI can be treated with medication or certain procedures. While not life-threatening, CVI can be associated with more serious conditions, including deep vein thrombosis, which can be fatal. To learn more, we spoke with Jose L. Trani, M.D., a board-certified vascular surgeon at Providence Swedish, who shares tips on recognizing the signs of this potentially serious health condition.
What is CVI and what causes it?
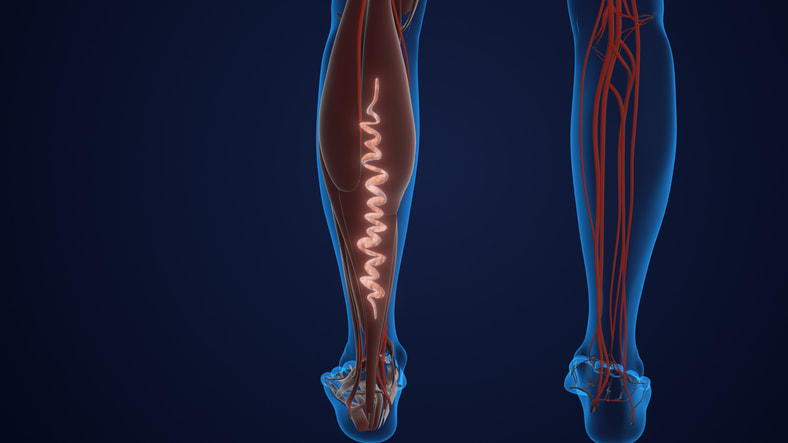
CVI is a disease that occurs when veins in your legs are damaged and can’t manage blood flow as well as they should. This makes it harder for them to return blood to your heart. With CVI, blood pools in your leg veins, increasing the pressure in them and in turn on your vascular system. CVI can happen due to damage in any of your leg veins, including your deep veins, which are large veins deep in your body that run through your muscle; your superficial veins, which are close to your skin’s surface; or your perforating veins, which connect your deep and superficial veins. Initial symptoms may be mild, but they can worsen over time and affect your quality of life or lead to serious complications.
With CVI, the valves in your legs are leaky, making it more difficult to return blood to your heart. When this happens, blood pools or collects in your legs, causing heaviness, tiredness, and swelling. This process can happen in any vein in your leg from ones just beneath the skin to those located deep in the muscles. Symptoms may present innocently but can worsen over time, affecting quality of life and occasionally leading to more serious issues.
What does CVI do to the body?
CVI slows down blood flow from your legs back up to your heart. Untreated CVI raises the pressure in your leg veins so much that your tiniest blood vessels, called capillaries, burst. This is what causes the reddish-brown color stains on the skin of people with CVI. This weakened skin is delicate, so these patients bleed easily if bumped or scratched. These burst capillaries are also associated with inflamed or damaged tissue in the lower legs. Venous stasis ulcers are a serious condition associated with CVI. These ulcers are open sores on your skin’s surface which don’t heal easily. They can become infected and cause a condition known as cellulitis, which can be extremely dangerous if not treated right away. CVI is not reversible, but there are pharmaceutical as well as surgical and non-surgical treatments — including anticoagulants, sclerotherapy and phlebectomy — that can help alleviate your symptoms.
CVI, through chronic swelling, has longstanding effects on the legs over time. The increased pressure allows fluid to leak out of blood vessels and into the surrounding tissue. This creates conditions where inflammation may develop. This inflammatory environment can cause small injuries to take much longer to heal than usual, often leading to specialist care to assist in wound healing. The tissue under the skin can become scarred and thickened. Finally, red blood cells that leak out of circulation along with the fluid become trapped there. As they die, the cells release iron, the oxygen carrying component, and this oxidizes, causing darkening of the skin.
DVT is the most common cause of CVI because the clots associated with DVT scar the vein’s tissue, damaging the valves and compromising their ability to efficiently return blood to the heart. Other causes can be congenital, meaning that you can be born with malformations in the leg or vein that affect vascular function or primary, meaning something happens to your veins that prevent them from working as they should. A vascular medicine physician can help you determine the cause of CVI.
Other causes are hereditary, meaning that if your parents or siblings have varicose veins that you have an increased chance of having them as well. This is because the veins and valves become weak and stretch over time. Finally, for women, pregnancy can lead to varicose veins and venous insufficiency. A vascular medicine physician can help you determine the cause of CVI.
What are some CVI symptoms I should look out for and how can I avoid or manage it?
CVI has a host of signs and symptoms. You should keep an eye out of them if you think you may be predisposed to the condition. They may include:
- Achy or tired legs.
- Burning, tingling or “pins and needles” sensation in your legs.
- Nighttime leg cramping.
- Reddish-brown skin stains.
- Swollen lower legs or ankles, especially after standing for a while or at the end of the day.
- Flaking or itching skin on your legs or feet.
- Leathery-looking skin on your legs.
- Open sores near your ankles. If they’re very painful, they may be infected, and you should see a doctor immediately.
To promote vein health in your legs even if you don’t suspect that you have CVI, be sure to exercise regularly, especially walking which promotes blood frow from your legs to your heart. Elevate your legs above your heart a couple of times a day. This can help reduce pressure on your leg veins. Your calf muscles play a vital role in keeping your blood moving up to your heart and throughout your body. And manage your weight, which also helps take pressure off your legs and your entire vascular system. And you can also consider compression therapy, which can help ease leg swelling and discomfort. Your physician can help you learn more about compression and if it’s right for you.
Learn more and find a physician or advanced practice clinician
The experts at Swedish Vascular Surgery can diagnose and treat a wide range of vascular disorders, and can help you determine the most effective and appropriate treatment for your condition.
Whether you require an in-person visit or want to consult a doctor virtually, you have options. Contact Swedish Primary Care to schedule an appointment with a primary care provider. You can also connect virtually with your provider to review your symptoms, provide instruction and follow up as needed. And with Swedish ExpressCare Virtual you can receive treatment in minutes for common conditions such as colds, flu, urinary tract infections and more. You can also use our provider directory to find a specialist or primary care physician near you.
Information for patients and visitors
Related resources
Understanding deep vein thrombosis (DVT)
Heart health advice for every age
Patient goes the distance for TAVR
Are you at risk for heart disease? Take this short quiz to learn more.
This information is not intended as a substitute for professional medical care. Always follow your health care professional’s instructions.
Providence Swedish experts in the media
Follow us on Facebook, Instagram and X.
About the Author
More Content by Swedish Heart & Vascular Team























