[5 min read]
In this article:
-
Swedish is home to the largest colon and rectal clinic in the Pacific Northwest.
-
Colorectal screenings, including colonoscopy, stool blood tests and ColoGard, save lives.
-
Watch the short video to learn about the causes of colon and rectal cancer, as well as risk, prevention and the importance of screenings.
-
Can you sing along to this song? If yes, then schedule your colonoscopy today.
Is it time for a colonoscopy?
Recent news about the untimely death of actor James Van Der Beek has brought colon cancer back into the spotlight. Van Der Beek was just 48 when he died of the disease on February 11, leaving behind a wife, six children and millions of adoring fans. Colorectal cancer is the No. 2 cause of cancer-related deaths in the United States. But it’s also one of the most preventable cancers.Van Der Beek, who was diagnosed in 2023, was a vocal advocate for colon cancer screenings and awareness. To learn more about how to prevent and treat colon cancer, we spoke with Lindsay Sceats, M.D., a colorectal surgeon at Swedish.
What is colorectal cancer
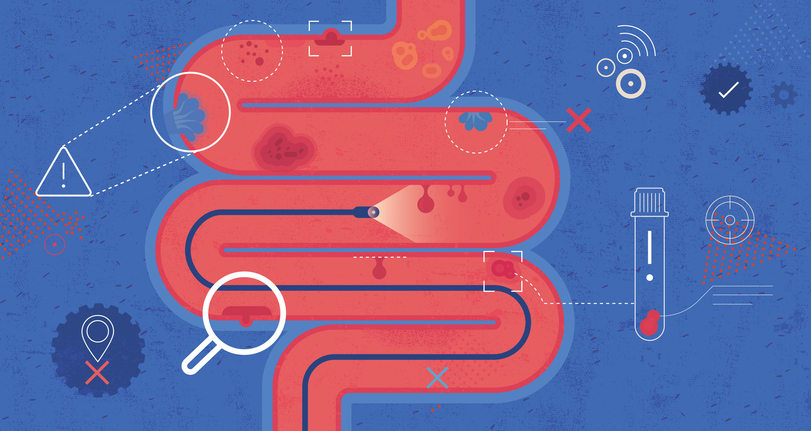
Colorectal cancer starts in the colon and rectum, is known as the large intestine. Typically, a small, noncancerous group of cells (called a polyp) forms in the lining of the rectum or colon. Some polyps are harmless, but others grow out of control and become colorectal cancer.
Removing any polyps in the colon or rectum as soon as possible is best. If they stay there, they may become cancerous, grow and spread to other organs, including the liver.
Treating colorectal cancer
Many patients undergo surgery to try to remove the cancer. How and if surgery happens depends on the stage of the cancer, the size of the tumor and where it’s located, and the patient is healthy enough to undergo surgery.
Precancerous polyps can often be removed with a colonoscope – the long, flexible tube and camera that’s used during a colonoscopy. This procedure is called a polypectomy. More advanced cancers may require more advanced surgeries and treatments to remove part of teh colon and the nearby blood vessels and lypmh nodes. Some patients need chemotherapy before or after surgery and possibly radiation.
Preventing colorectal cancer
Colorectal cancer can be devastating. But the good news is that most cases are preventable. The best prevention for colorectal cancer is regular screenings. There are several screening options, including fecal occult blood tests, stool DNA tests and colonoscopies. Colonoscopy is considered the gold standard of colorectal screening tools.
With a colonoscopy, doctors can find polyps early and remove them – before they become cancer. Treatments for colorectal cancer are most effective when the cancer is caught early. And a colonoscopy helps find problems at the earliest stage possible.
When to get a colonoscopy
In the past, the recommendation was to start having colonoscopies at age 50. Recently, more younger people have been getting colorectal cancer, so the American Cancer Society now recommends getting your first colonoscopy at age 45, and then every 10 years until you’re at least 75.
The best place to start is to talk to your provider about your risk of colorectal cancer. Your provider may suggest that you start getting coloscopies at a younger age or more frequently if you have certain risk factors for colorectal cancer. Examples include:
- Having a family or personal history of colorectal cancer or polyps.
- Having inflammatory bowel disease (IBD).
- Having genetic syndromes, such as Lynch syndrome or familial adenomatous polyposis (FAP).
- Being overweight or obese.
- Eating a lot of red meat.
- Smoking or drinking a lot of alcohol.
But isn’t getting a colonoscopy…terrible?
You may have heard stories from relatives or friends about getting a colonoscopy. Maybe their comments have made you delay screening. A colonoscopy may not be fun, but for most people the procedure is pretty routine and can reduce your risk of colorectal cancer by up to 70%. Still, we know that rumors and myths can keep you from your screening, so let’s talk about it.
What people say: “I don’t need to have a colonoscopy if I don’t have any symptoms.”
The truth: A colonoscopy is all about prevention. By the time you have symptoms of colorectal cancer, the cancer has been in your body for a while and may limit effective treatment options. The goal of regular screening is to prevent the cancer altogether, so when you get a colonoscopy, you probably won’t have any symptoms.
If you have one or more of these symptoms, you should talk to your provider right away:
- Bleeding from the rectum
- Pain when using the bathroom
- Weight loss (without trying)
- New constipation, diarrhea, or changes to your normal bowel habits.
What people say: “The prep is the worst and makes you gag.”
The truth: We won’t lie. Preparing for a colonoscopy isn’t the most enjoyable activity. But most people also agree that’s it not the worst thing in the world. These steps are usually part of “the prep”:
1. You’ll get a prescription laxative (“prep”) with instructions a few days before your colonoscopy. The prep is usually a liquid provided in two containers. It helps your body get rid of waste, so your provider can clearly look at the inside of your colon and rectum during the colonoscopy.
2. For the full day before your colonoscopy, you’ll eat clear liquids only – such as broth, Jell-O or popsicles.
3. You’ll drink part of the prep the night before, usually at around 6 p.m. You don’t have to chug the prep, and you can mix it with clear liquids like ginger ale or Gatorade if you prefer.
4. You may have to wake up really early to finish the rest of the prep. You must finish it four hours before your colonoscopy, which will probably be scheduled in the morning.
What people say: “The colonoscopy hurts.”
The truth: Most people get a colonoscopy with sedation. This means you feel like you’re asleep, but you don’t get general anesthesia from an anesthesiologist (unless it’s a special case). The procedure shouldn’t hurt. Some people report feeling some cramping and minor discomfort.
The procedure itself takes about 30 minutes. When you wake up, you have some time to recover. After that, you’re free to leave as long as you have someone to drive you home.
Watch the video to learn about the importance of colonoscopies and the early detection of colon cancer from Dr. Lindsay Sceats, a Providence Swedish colon and rectal surgeon
Find a physician or advanced practice clinician (APC)
If you or a loved one want to learn more about cervical cancer or treatment, the experts at Swedish Cancer Institute are here for you. To learn more, visit our website, or to speak with someone or make an appointment, call 1-855-XCANCER.
Whether you require an in-person visit or want to consult a doctor virtually, you have options. Contact Swedish Primary Care to schedule an appointment with a primary care provider. You can also connect virtually with your provider to review your symptoms, provide instruction and follow up as needed. And with Swedish ExpressCare Virtual you can receive treatment in minutes for common conditions such as colds, flu, urinary tract infections, and more. You can use our provider directory to find a specialist or primary care physician near you.
Information for patients and visitors
Additional resources
Did you know that colon cancer is on the rise among younger adults? Screening is key to prevention.
Get the scoop on your poop and what it says about your health
This information is not intended as a substitute for professional medical care. Always follow your health care professional's instructions.
Follow us on Facebook, Instagram and X.
The Providence app offers world-class health care with human connection
About the Author
More Content by Swedish Cancer Team





















